Software to Read X-ray Class Ii Device? Fda
During 2019, many AI healthcare companies announced FDA clearance for their medical device - this ofttimes considers AI radiology software. What does information technology actually mean when a company claims their artificial intelligence software is approved by the FDA? Why is this important? How does the FDA regulatory pathway for artificial intelligence radiology software currently work? And where do CADe and CADx versus AI fit in this story? Well, for a start, if y'all want to employ the software in clinical context, information technology is mandatory. All the same, as is oftentimes the case with rules, they exist for a reason. An FDA stamp of approving confirms the medical device in question has been extensively vetted by an authorization that is specialized to do so. In other words, information technology provides certainty on the safety and efficiency of the device. The FDA has an extensive review process to make up one's mind whether a medical device is prepare for clinical utilise. Which concrete steps the process contains is determined by what blazon of device is up for blessing - a medical device, a device that does non claim to fulfill a medical purpose, or an investigational device. Software that meets the definition of a medical device is regulated past the FDA. This ways that software intended to be used for diagnosis, prevention, monitoring, treatment, or alleviation of a disease or injury may only be marketed for clinical use after information technology complies with FDA regulation. The FDA has ready a organization in which devices, including software, have to be proven safe and constructive for their intended use in diverse areas such as (datasets for) algorithm validation, blueprint, (stand up-alone and clinical) operation, usability, and also cyber-security. Furthermore, not only the products need to comply with FDA regulation, but too manufacturers themselves are required to operate according to the Quality System Regulations. This obligates manufacturers to take processes in place for controlled bug resolution, incident reporting, standardized design processes and overall risk direction. For software that does not fulfill a medical purpose, FDA regulations are not applicable. This ways no evaluation of the clinical performance and no requirements on proper software design and cybersecurity measures; basically, no bank check that the device can fulfill its intended use safely and effectively. Such algorithms may be very suitable to utilise in a enquiry setting and can offering additional features supporting enquiry fairly, such as majority export of data. However, they are non necessarily meant, nor designed to exist as robust, prophylactic, and constructive as is required for clinical use (i.e. provide information that is used for individual patient management). Some hospitals, mainly academic ones, utilize such inquiry software. This is ordinarily adult in house and should be deployed for scientific research just. For example, software that provides volumetric data past automatically segmenting brain structures on MRI images can be a valuable addition to a research project. Software falls into the category of "investigational device" if information technology is part of a clinical trial to be evaluated on clinical operation with the purpose of obtaining FDA approval. This means the software is non cleared for support of clinical conclusion making just yet. Outcomes of the clinical trial first accept to prove (or disprove, of class) that the device accurately provides the correct information. However, performing a retrospective study, in which the software device is non directly used for clinical conclusion making, often offers a more straight-forward approach for obtaining regulatory clearance.1 An example of a study with an investigational device is stroke detection software that is integrated into the radiology workflow and used to diagnose patients, while other patients presenting with stroke related symptoms are diagnosed without the software. The stroke detection software volition exist part of a clinical trial of which the purpose may be to compare diagnosis decisions made with and without the software. It might be a flake of an anti-climax, but whether a device belongs to any of the three categories discussed to a higher place does non accept annihilation to practice with whether the product is AI-based. A medical device can use artificial intelligence techniques, simply like a "non-medical device" or an investigational device. But bear with u.s., nosotros volition go to the AI part in a bit. The FDA has determined over 1700 different generic types of devices and assigned those a production code and a classification as class I, Ii, or Iii. This nomenclature is based on the chance the product poses and its intended apply. The higher the take chances of your product, the more stringent the procedure to get it FDA approved. If a medical device searching clearance fits the criteria of an existing product code that is assigned to Class I or Two, completing what is called the 510(k) program volition provide FDA clearance for the device .2,three The process is relatively straight forward: beginning, identify an FDA cleared device that is substantially equivalent to your device (this is called the predicate device), secondly, prove that the device performs at least at the aforementioned safe and effectiveness level. Again, at that place is no reason such a device cannot contain AI-technology. However, as many AI-techniques that are presently implemented in medical devices are relatively new and practice not take an intended employ that has been cleared in a previous device, chances are high that the device is non eligible for the 510(g) pathway. This immediately assigns the device to Class III. Class II products are usually depression patient risk, for example, powered wheelchairs, or devices with established techniques and materials that do not have life support functions, such as an 10-ray mammography organization or Ophthalmic organisation prototype management. Class III devices normally sustain or back up life, or nowadays potential unreasonable chance of disease or injury to the patient. Undisputed devices in this category are all things implantable, such every bit pacemakers and stents. A device can be assigned to form III in two ways. First, when it fits one of the generic device groups as described past the FDA that already take a product code assigned and are adamant to exist class Iii. A second scenario is when the FDA has not coded and classified the device blazon nevertheless. Then information technology is a new "device type" and there is no product code available. The FDA automatically assigns the device to grade Iii. This is the instance for many new healthcare concepts, including well-nigh AI-based software. This will require a device to get through the more extensive process of Premarket Approval (PMA) which, if successful, will lead to FDA approval prior to marketing your device. A PMA demands an applicant to provide "valid clinical information and scientific analysis". 4 In other words, clinical investigations, such every bit clinical trials, must exist proved in add-on to the technical and non-clinical studies which are already required for class I and II devices. Not only is the FDA neb for the PMA process significantly college than for the 510(k) procedure, but the required clinical trials are usually expensive as well equally time consuming. Furthermore, extensive communication with the FDA tin can be expected throughout the review process, requiring a vast amount of resources and time to blessing - significantly more is necessary for a 510(k) process. For all those smaller companies out there that do not have the resources to cover the full course of a PMA process, there are two alternative approaches still open later existence categorized in grade III. Selection 1: track down a predicate device. If yous succeed at finding a medical device with the same intended apply - which is substantially equivalent in safety and effectiveness - there is a big chance that product serves as a suitable predicate device for substantial equivalence decision. Significant that the product is similar enough to the medical device upward for approval to make it fit class Two and therefore able to be cleared by completing a 510(k) procedure. Selection 2 requires y'all to convince the FDA that the risks your device may put on patients is acceptable enough for the less stringent review pathway. This is done by sending in for review what is called a De Novo classification request.5 For this, yous prepare technical documentation that contains a detailed description of the device, clinical and non-clinical performance tests, usability, and risk management activities. This is very like to the way you prove safety and effectiveness in a 510(k) file. Furthermore, all the patient risks and patient benefits of the device have to exist explained, including their mitigations, and propose special controls to ensure that the production is safe and effective in use. If the De Novo is granted, the device is categorized every bit Class II and the device group is now eligible for the 510(m) pathway with your device as a predicate device. If the FDA rejects your De Novo, there is no selection left but to get for the more than excessive PMA process. The route of going through a De Novo process is really a path that is oft chosen by manufacturers seeking approval for their new AI-based devices. CADe and CADx, standing for Reckoner Aided Detection and Computer Aided Diagnosis, respectively, frequently create confusion when talking about AI in healthcare. The definitions the FDA adheres to are as follows: a radiological CADe device is "intended to identify, marking, highlight or otherwise straight attending to portions of an paradigm […] that may reveal abnormalities during estimation of images by the clinician." A CADx device is "intended to provide information beyond identifying […] abnormalities, such as an assessment of illness." Whenever software is not intended to highlight an abnormality, information technology is not considered a CADe nor a CADx device. For instance, segmentation of brain structures is not considered CADe, while the detection of a tumor candidate is. An algorithm that adds information on tumor grade would make it a CADx device. So how does this relate to the unlike classes? In general, radiological CADx software will nearly likely fall nether Class 3 at the fourth dimension of writing, while radiological non-CADe software may notice a Grade 2 predicate device in the Image Analysis System (LLZ) product code. Radiological CADe software can be both course II or form III, this is adamant by the "regular process". As shortly equally the device detects abnormalities, it is a CADe. Examples are CT lung nodule analysis and chest X-ray analysis. The category of CADe devices falling in Class II increases with every granted DeNovo. Lastly, there is a specific product code for devices that include borderline radiological CADe/CADx functionality. This is a wild card the FDA can play if the device is sort of CADe or CADx, merely non really. All the same no word of AI. Not-CADe, CADe, and CADx software can all utilize artificial intelligence technology. CADe and CADx software tend to include AI more often, merely a non-CADe device might only likewise be deep learning-based. The FDA has published 2 specific guidance documents for evaluation of CADe devices. These documents provide management on requirements for dataset drove, algorithm validation, setting up reader studies, and more - all very useful for AI radiology software.6,7 Frankly speaking, not that much. Currently, the FDA works with guidelines that were adult in a pre-AI era. Almost of the fourth dimension, this is not a problem. Equally long as the manufacturer can provide detailed information on how the algorithm was adult and evidence that information technology is suitable for safe and effective apply. In instance of and so-called continuous learning algorithms, i.due east. algorithms that keep learning and therefore changing while existence used in the dispensary, the example becomes a bit more hard. The FDA is working on guidelines covering this situation. To read more well-nigh this, cheque out our blog on how the FDA is planning to bargain with continuous learning. Whether the FDA categorizes a device as a class II or III, or whether it is labeled CADe or CADx does not make a departure for how to employ the device in the clinic. Fifty-fifty the presence of AI-based algorithms (or lack thereof) is non relevant. If you desire to use a medical device in clinical practice, the merely important factor is that information technology is cleared or approved to be used for the task y'all are planning to use information technology for. Are you looking for software to back up your inquiry? And so non-approved algorithms might be able to do the task simply fine. They are ordinarily cheaper and easier to customize, which might exist of do good to the research. However, this is only possible because they are not tested for safety and effectiveness as extensively as software that is cleared or approved for clinical utilise. This is something to consider before making your selection. Why is it important that AI radiology software receives a nod past the FDA?
How does the FDA currently deal with AI radiology software?
Type one: A medical device
Type ii: The device does not merits to fulfill a medical purpose, e.thou. inquiry software
Type three: An investigational device
So where does AI fit in this story?
The software classifies as a medical device. What's adjacent?
Form I and II
Class III
Thought to be class III, but institute to be form II
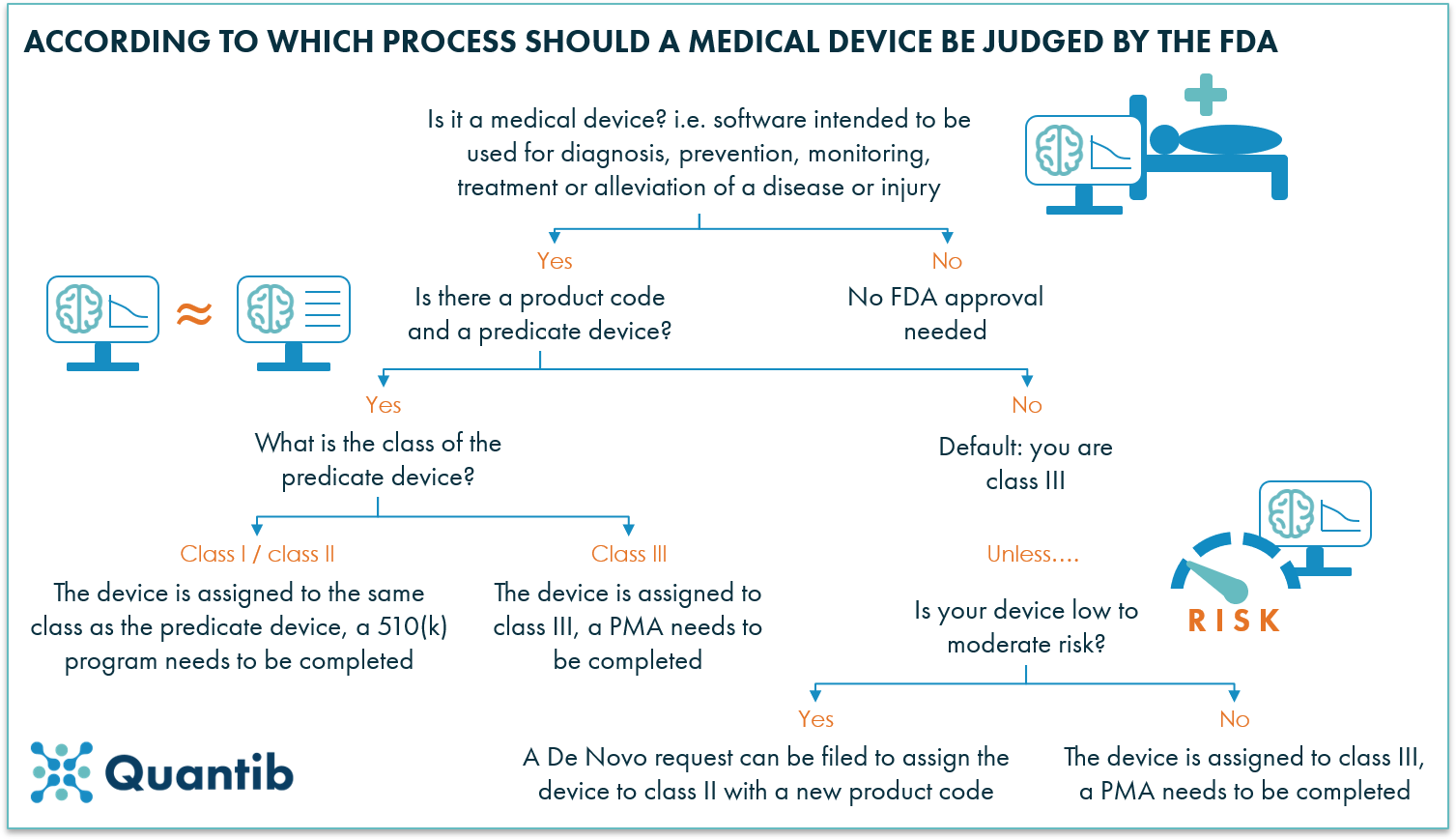
Figure 1: The FDA regulatory path consists of many processes. The figure above explains which process to follow, depending on the state of affairs. 
How about radiological CADe and CADx vs AI?
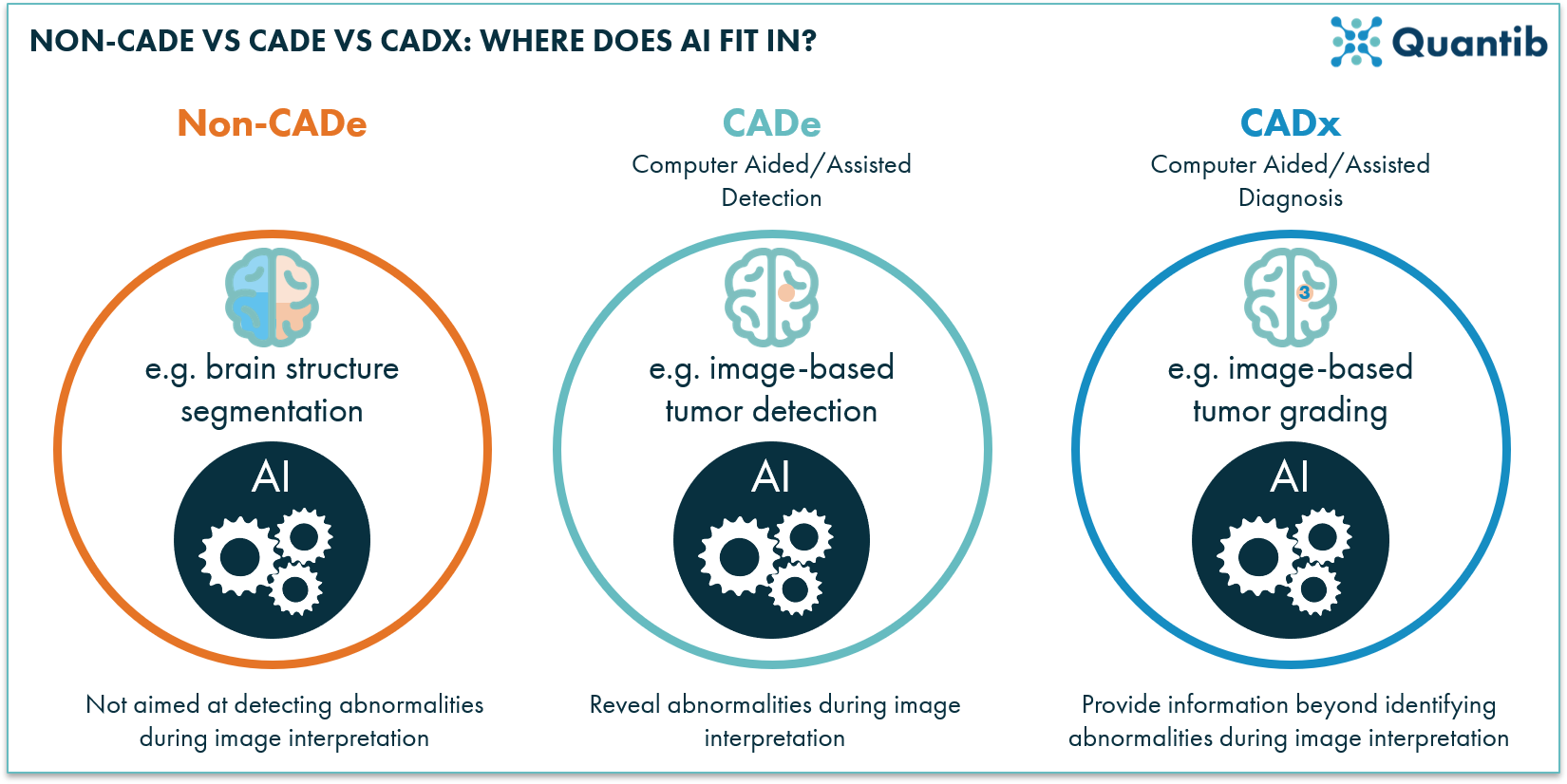
Figure 2: Non-CADe, CADe, and CADx - how practise these types of products chronicle? All can be based on AI technology, but they have a unlike function. And so then what DOES the FDA say about AI?
As a doc, what should you pay attention to?
Bibliography
Source: https://www.quantib.com/blog/a-101-guide-to-the-fda-regulatory-process-for-ai-radiology-software